It has been widely reported that the number of Americans being diagnosed with major depressive disorder is increasing. A certain segment of folks with depression does not find relief with antidepressant medications and talk therapy, falling into the category known as treatment-resistant depression. Individuals with this ongoing illness often lose interest in activities they once enjoyed, have difficulty interacting with others, and may even have thoughts of suicide.
Fortunately, Sheppard Pratt has a one-of-a-kind center to bring hope to people who have been suffering. The Institute for Advanced Diagnostics and Therapeutics was established to provide expert clinical care through established and newly developed treatments.
Success with TMS
One treatment available through the institute is transcranial magnetic stimulation (TMS), which uses magnetic pulses directed at specific areas of the brain to generate small electrical currents. To patients, these pulses feel like a light tapping sensation. The electrical currents are believed to activate changes that produce beneficial neurotransmitters like serotonin, norepinephrine, and dopamine.
Patricia Carlson, MD, is the service chief of Sheppard Pratt’s TMS program. “TMS is a great option for people who haven’t found relief from medication or therapy in the past,” she says.
This treatment has few, if any, side effects, with the most common being a headache that usually goes away in the first week of treatment. There are no restrictions or lingering effects. “People can drive, work, or go to school right after a TMS treatment,” Carlson says.
Patients must be consistent. Twenty-minute treatments are given daily, Monday through Friday, for six weeks. Patients tend to notice improvement around the third or fourth week. Dr. Carlson mentions that TMS, when paired with talk therapy, could be used instead of antidepressant medications in some cases. And treatment sessions may be repeated after several months if a patient notices their mood shifting.
Today’s ECT
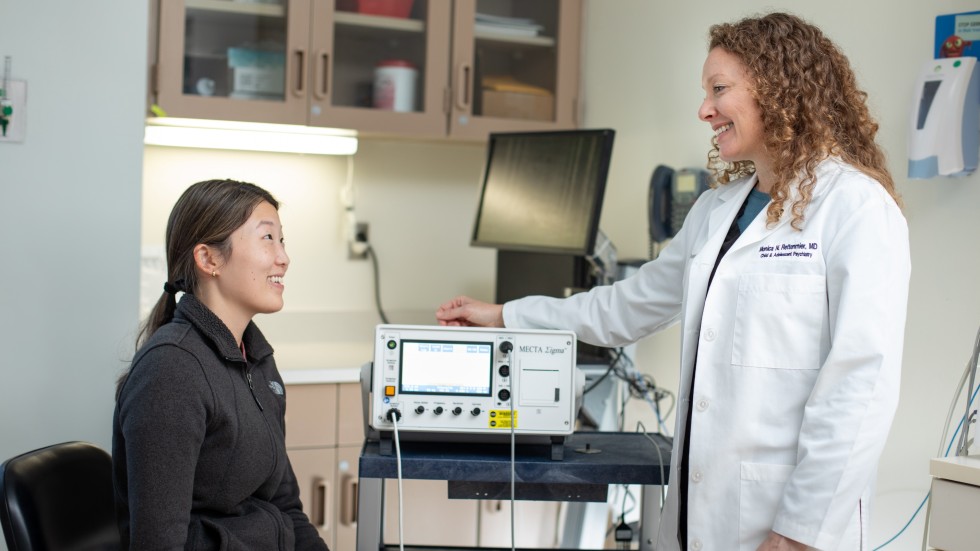
Treatment-resistant unipolar and bipolar depression can be treated with electroconvulsive therapy, or ECT. Used since the 1930s, ECT has been refined and improved for patient safety and comfort. “It’s not nearly the same experience patients had in the 1950s and 60s,” says Monica Rettenmier, MD, child and adolescent psychiatrist and ECT service chief for Sheppard Pratt. “It is much more comfortable and with far fewer side effects. Patients undergo psychiatric evaluation before treatment to ensure they are good candidates for the procedure. Then, they are put under anesthesia while their brain is stimulated with mild electrical impulses.
“Depictions of ECT from movies and TV shows of the past give the public a horrible impression of what the treatment is like. Patients are no longer subjected to continuous current, and the treatment session is painless.” Dr. Rettenmier adds that while there are some side effects from the treatment, such as fatigue and memory fog, the benefits for a patient can be significant.
An initial treatment series, typically eight to 14 treatments, takes place a few days a week for up to five weeks, says Dr. Rettenmier. “The number of treatments depends on the individual, the length of the acute depressive episode, and how deeply rooted the illness is.”
Patients experience a gradual improvement and are encouraged to continue medication and talk therapy. “Although patients typically do not immediately feel amazing, I have seen it happen,” says Dr. Rettenmier. “Rather, patients may notice that they are sleeping better or don’t immediately feel hopeless when they wake up. It’s a slow lifting of those depressive symptoms.”
Dr. Rettenmier adds that you don’t have to suffer from depression for a long time before trying ECT. “If you have concerns about your depression, reach out to your provider to ask them about ECT,” she says.
Like TMS, patients can resume sessions if their depression returns after the initial course of treatment.
The future of psilocybin
Researchers at Sheppard Pratt are also studying a synthetic version of the psychedelic compound psilocybin for treatment-resistant depression and other mood disorders. “We are leading the way in looking at novel treatment for a variety of disorders and for people who are not benefiting fully from standard treatments of care,” reports Tammy Miller, PsyD, clinical psychologist and lead psychotherapist for the psilocybin research trial. She and other researchers believe that this could be a revolutionary treatment for depression and other disorders, such as anorexia nervosa, obsessive-compulsive disorder, and PTSD.
“We are seeing that the synergy of the psychedelic drug—which is unique and unlike any standard mental health drug—together with psychological support is opening doors for patients in ways that current treatments are not,” says Dr. Miller.
During treatment, each study participant is given a dose of psilocybin and then monitored by a psychiatrist and a specially trained therapist who help the patient work through the feelings and thoughts that the drug invokes. “It’s a process that lasts six hours,” Dr. Miller explains. “The drug seems to be able to get underneath all of the emotions, create new neural pathways, and heal injuries.
But we discourage people from taking psilocybin outside of a medical setting, especially if they have a mental illness. If you seek out services through programs like ours or other clinical research trials, you can get safe, effective care.”
So far, many study participants have not had to resume antidepressant medications following psilocybin treatment, although they are encouraged to continue talk therapy.
“More than 30% of the participants who received a single dose of psilocybin were in remission the week after, and three months after, that single dose,” says Dr. Miller.
Hope is here for depression
If you or a loved one is dealing with depression, Sheppard Pratt is here to help.